
What is CAR T-cell therapy, and what does it mean for the future of cancer treatment?
Blood cancer is the third biggest cancer killer in the UK. However, a revolutionary immunotherapy treatment known as known as CAR T-cell therapy (Chimeric Antigen Receptor T-cell therapy) has brought renewed hope to blood cancer patients and the medical world alike.
Dubbed the ‘5th pillar of cancer treatment’ by many (following surgery, chemotherapy, radiotherapy and targeted therapies), CAR T-cell therapy is now available for eligible patients in the UK.
To help shed some light on this groundbreaking therapy, one of the UK’s leading experts on CAR T-cell therapy - Professor Stephen Mackinnon, Chair of the HCA Healthcare UK Blood Cancer Board has provided an overview on what CAR T-cell therapy is, how it works, and how it could transform the future of cancer treatment on a global scale.

What is CAR T-cell therapy?
“CAR T-cell therapy is a revolutionary new type of cancer therapy for blood cancer patients. ”
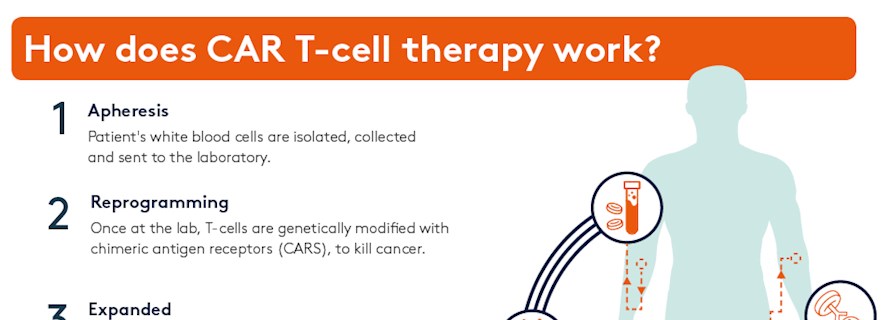
CAR T-cell therapy is a revolutionary new type of cancer therapy for blood cancer patients. The name refers to T-cells which have been modified with chimeric antigen receptors (CAR).
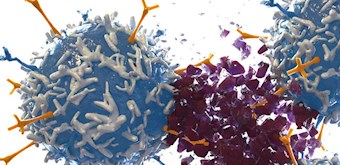
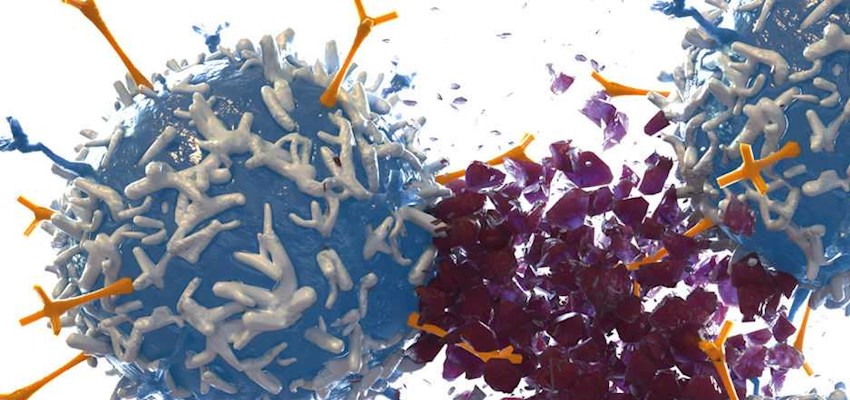
T-cells are a type of white blood cell which play a vital role in the immune system - orchestrating the immune response and killing cells infected by pathogens. During this process T-cells use their protein receptors to latch on to antigens found on the surface of other cells and examine them; the T-cell will move on if the examined cell is healthy or, when a diseased or cancer cell is discovered, T-cells release killer chemicals to destroy the abnormal cell. Unfortunately, cancer has the ability to evade and fool our immune system. It can do this by disguising itself as a healthy cell or by creating multiple abnormal antigens on its surface which prevent T-cell receptors latching on– giving the disease a chance to spread.
With CAR T-cell therapy, modified T-cells are specifically designed to strengthen and harness the immune system’s inherent cancer eliminating powers, adding new targeted receptors designed to seek, attach to and destroy cancer cells which may have previously gone undetected.
Following this, the separated T-cells are transported to a lab where they are engineered to express personalised and targeted CARs that recognise cancer cells, turning them into ‘CAR T-cells’.
These modified T-cells are then grown and expanded in a lab and millions of them are infused back into the patient following a short course of conditioning chemotherapy. Once the modified T-cells are back in the patient’s bloodstream their new receptors enable them to latch onto a specific antigen found on the patient’s tumour cells and destroy them.

How is the CAR T-cell therapy different to traditional immunotherapy?
Who is suitable for CAR T-cell therapy?
Launching this spring at HCA Healthcare UK, CAR T-cell therapy will initially be available to patients with diffuse large B-cell lymphoma, primary mediastinal large B-cell lymphoma and transformed follicular lymphoma, with plans to extend the offering to other blood cancers over the coming months. We are excited to provide this innovative treatment to our patients in our JACIE-IEC accredited units.


Is CAR T-cell therapy effective?
What does the future hold for CAR T-cell therapy?
Researchers are also currently working on a similar concept to CAR T-cell therapy for the treatment of solid cancer tumours (NAR T-cell therapy). This is another big step on, and it’s likely that the next decade will be highly transformative for cancer treatment.
The Leader - Issue One
Discussing advances in medicine - from the UK's healthcare leaders
